CENTERED BODYWORK- STRUCTURAL INTEGRATION, CRANIOSACRAL AND ORTHOPEDIC MASSAGE
|
Oregon has initiated a massive effort to help healthcare providers help their patients reduce pain and reduce opioid and other painkiller addiction. I've pulled together some resources for clients who have some continuing pain despite "successful" treatment. Sleep, diet, emotions, exercise, stress and more all effect the amount of pain people experience, in fact whether pain is experienced at all.
The research shows there is only a modest connection between tissue dysfunction and the amount of pain. Many people have tissue dysfunction and no pain. Others have minimal tissue dysfunction and disabling levels of pain. The brain is a the key moderator to pain and it can be supported to sense less pain. That doesn't main the pain is not real, after all pain is in essence sensation. If you feel the pain, the pain is absolutely real. It's just that in some cases the pain is disporportionate to the threat. Perhaps there is no more threat at all to the body's systems and the pain is still firing anyway. Here are some resources to study if you have persistent pain:
0 Comments
Low back pain is one of the most common types of pain and self care is so important in our sedentary culture. I created this sequence of gentle Qi Gong movement practices for low back wellness and for helping with existing mild low back pain. A healthy, mobile spine is crucial as you age because the nerves that come out of your spine innervate your organs! Please check in with your doctor before beginning any exercise program, especially if you have any medical issues with your spine or moderate to severe back pain. The video starts off easy and integrates more challenging movements as the video progresses. Please skip any movements that cause pain. Enjoy!
By Dr. Gabe Mirkin, posted 2/2/2019
When I wrote my best-selling Sportsmedicine Book in 1978, I coined the term RICE (Rest, Ice, Compression, Elevation) for the treatment of athletic injuries (Little Brown and Co., page 94). Ice has been a standard treatment for injuries and sore muscles because it helps to relieve pain caused by injured tissue. Coaches have used my "RICE" guideline for decades, but now it appears that both Ice and complete Rest may delay healing, instead of helping. In a recent study, athletes were told to exercise so intensely that they developed severe muscle damage that caused extensive muscle soreness. Although cooling delayed swelling, it did not hasten recovery from this muscle damage (The American Journal of Sports Medicine, June 2013). A summary of 22 scientific articles found almost no evidence that ice and compression hastened healing over the use of compression alone, although ice plus exercise may marginally help to heal ankle sprains (The American Journal of Sports Medicine, January, 2004;32(1):251-261). Healing Requires Inflammation When you damage tissue through trauma or develop muscle soreness by exercising very intensely, you heal by using your immunity, the same biological mechanisms that you use to kill germs. This is called inflammation. When germs get into your body, your immunity sends cells and proteins into the infected area to kill the germs. When muscles and other tissues are damaged, your immunity sends the same inflammatory cells to the damaged tissue to promote healing. The response to both infection and tissue damage is the same. Inflammatory cells rush to injured tissue to start the healing process (Journal of American Academy of Orthopedic Surgeons, Vol 7, No 5, 1999). The inflammatory cells called macrophages release a hormone called Insulin-like growth Factor (IGF-1) into the damaged tissues, which helps muscles and other injured parts to heal. However, applying ice to reduce swelling actually delays healing by preventing the body from releasing IGF-1. The authors of one study used two groups of mice, with one group genetically altered so they could not form the normally expected inflammatory response to injury. The other group was able to respond normally. The scientists then injected barium chloride into muscles to damage them. The muscles of the mice that could not form the expected immune response to injury did not heal, while mice with normal immunities healed quickly. The mice that healed had very large amounts of IGF-1 in their damaged muscles, while the mice that could not heal had almost no IGF-1. (Federation of American Societies for Experimental Biology, November 2010). Ice Keeps Healing Cells from Entering Injured Tissue Applying ice to injured tissue causes blood vessels near the injury to constrict and shut off the blood flow that brings in the healing cells of inflammation (Knee Surg Sports Traumatol Arthrosc, published online Feb 23, 2014). The blood vessels do not open again for many hours after the ice was applied. This decreased blood flow can cause the tissue to die from decreased blood flow and can even cause permanent nerve damage. Anything That Reduces Inflammation Also Delays Healing Anything that reduces your immune response will also delay muscle healing. Thus, healing is delayed by: • cortisone-type drugs, • almost all pain-relieving medicines, such as non-steroidal anti-inflammatory drugs like ibuprofen (Pharmaceuticals, 2010;3(5)), • immune suppressants that are often used to treat arthritis, cancer or psoriasis, • applying cold packs or ice, and • anything else that blocks the immune response to injury. Ice Also Reduces Strength, Speed, Endurance and Coordination Ice is often used as short-term treatment to help injured athletes get back into a game. The cooling may help to decrease pain, but it interferes with the athlete's strength, speed, endurance and coordination (Sports Med, Nov 28, 2011). In this review, a search of the medical literature found 35 studies on the effects of cooling . Most of the studies used cooling for more than 20 minutes, and most reported that immediately after cooling, there was a decrease in strength, speed, power and agility-based running. A short re-warming period returned the strength, speed and coordination. The authors recommend that if cooling is done at all to limit swelling, it should be done for less than five minutes, followed by progressive warming prior to returning to play. My Recommendations If you are injured, stop exercising immediately. If the pain is severe, if you are unable to move or if you are confused or lose even momentary consciousness, you should be checked to see if you require emergency medical attention. Open wounds should be cleaned and checked. If possible, elevate the injured part to use gravity to help minimize swelling. A person experienced in treating sports injuries should determine that no bones are broken and that movement will not increase damage. If the injury is limited to muscles or other soft tissue, a doctor, trainer or coach may apply a compression bandage. Since applying ice to an injury has been shown to reduce pain, it is acceptable to cool an injured part for short periods soon after the injury occurs. You could apply the ice for up to 10 minutes, remove it for 20 minutes, and repeat the 10 minute application once or twice. There is no reason to apply ice more than six hours after you have injured yourself. If the injury is severe, follow your doctor's advice on rehabilitation. With minor injuries, you can usually begin rehabilitation the next day. You can move and use the injured part as long as the movement does not increase the pain and discomfort. Get back to your sport as soon as you can do so without pain. Editor's Note: In myofascial release, we break up collagen fibers that are excessive. It may be useful to ice so that the body does not bring back more collagen to the area immediately after treatment. This is why I do not recommend hot baths after myofascial release and do recommend ice if the area is too sore after treatment. Unlike an injury, we are actually clearing out the cobwebs of collagen and ideally not doing damage to healthy tissues. 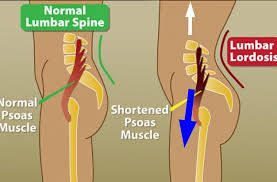
The psoas is a large muscle that reaches from the spine (just above the belly buttom) down through the abdomen and across the hips to attach on the inner, upper femur. The psoas responds to fear to pull the body into a protective, curled up position. It also becomes inflexible from sitting, running, cycling, driving and more. It can cause issues in the low back, hips, sacrum, SI joints and pelvis primarily.
Here's a few ways to release your psoas gently so that it doesn't spasm or recoil. Make sure you release both sides so you feel or see the same amount of flexibility on both sides, which likely means less time on the more flexible side. Make sure to not overdo it. The psoas responds to less not more stretching and be gentle! CNN recently posted two articles highlighting both the newness of our understanding of fascia and its importance. Fascia is proposed to be the largest organ in our body. It holds and connect everything together. Scientists now believe what many myofascial, craniosacral and stuctural integration therapists know, fascia can also cause pain, injury, premature aging and lack of mobility.
As we manipulate fascia, it becomes more flexible, nourished and mobile from the tissues around it. However, as we manipulate fascia we are also applying friction to muscles, releasing impinged nerves and restricted blood vessels, and moving fluids. It's because of this complexity of the human body that we may never know exactly why fascial release and massage work at any given point in treatment. However, there are limited studies on fascia:
To understand more about this increasingly important organ, read:
Massage is the number one most effective treatment for carpal tunnel prevention and treatment. However, if you work in an office or have another hand heavy usage job, you may need more regular care than you can afford with a massage therapist due to the repeated strain on your body.
I found this video instruction on carpal tunnel self massage and it pretty much exactly what I've been teaching my clients to do for years. For reference, you can also test yourself for carpal tunnel but its best to see a doctor and rule out other causes of numbness, pain and tingling in the hands.
In the age of tech and information, many people forget their bodies and are totally in their heads. Yet there is a reason to focus on your body even if you only care about your mind. If you want an optimally functioning brain, exercise is key to brain health.
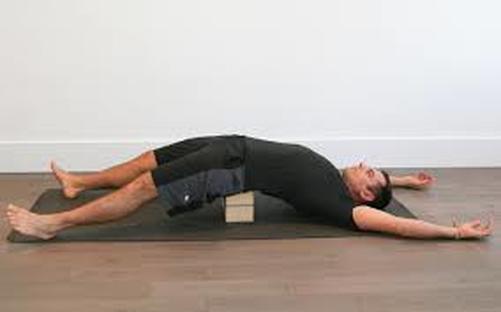
Excerpt from an article by LMT Tracy Laval posted July 16th, 2018 on the Idea Crucible Read the full article here. Below are 5 simple and practical ways to calm your nervous system to reduce the tension in your jaw by deactivating your defensive responses. I use this same approach regularly in my clinic where I specialize in TMJ jaw pain. I give these correctives to my clients in my clinic and I do them myself daily. They are effective and easy to use and a great place to start. 1. Slowly alternate breathing in and out of your nostrils: Why? Stretching out your exhale slows down your heart rate. This calms your nervous system. Slowing your breathing has the fastest affect on calming your nervous system. Alternating your breath out of each nostril has the added benefit of linking your left brain with your right brain for better communication and balance in your nervous system. Instructions: Set a gentle alarm for 11 mins (I use my phone). Close your eyes. Close your mouth. Breathe in and out through your nose. With one hand raised to your nose, press your thumb into the side of your right nostril, just below the bone halfway down your nose. Inhale through your left nostril, breathing slowly and deeply. At the end of the inhale press your ring finger from the same hand into the side of the left nostril and remove your thumb. Exhale slowly from the right nostril. Stay in this position and inhale through the right nostril. At the end of the inhale press your thumb into the side of your right nostril and exhale from the left nostril. Repeat until your alarm rings indicating you to stop. Do this daily. Do it when you first wake up or whenever you want a clear head for thinking or more energy (like after lunch or late afternoon). You might find it energizing. 2. Laying Down Chair: Why? Because this relaxes your psoas muscle which is deeply connected to your nervous system. If it is chronically tight it will have an agitating effect on your nervous system and trigger your flight or fight stress response. Instructions: Lay on the floor on your back in front of a chair with the seat facing you,(or footstool or couch). Bend your hips and knees to 90 degrees each so that your calves are resting on the seat of the chair. Allow the chair to support your lower legs completely, checking to see that you aren’t using your leg muscles or hip muscles to hold your legs up. Allow your leg and hip muscles to relax and for your belly to become soft (you are aiming for your belly to feel like it’s made of honey or jelly). This relaxes your nervous system. Rest here for 20 mins. Do daily anytime (before bed or a meal is best). It will help your sleep and digestion. 3. Back your chin up Why? Because your head position affects the amount of jaw tension you have. Your jaw muscles contract to help your neck muscles hold your head up against the downward pull of gravity. When your chin is forward, away from the centre of your body, this strains and compresses the area at the top of your neck where vital nerves and blood supply feed your brain reducing blood flow and nerve function. It’s also a tremendous amount of work for your body to balance your head out in front of your body, suspended against the downward pull of gravity. Your head weighs around 12 pounds. For every inch your head moves forward away from your midline it adds an extra 10 pounds. For every inch! How many inches is your head forward when you are looking at your phone, at your computer or driving? It’s normal to get drawn into what we are doing but it’s not ideal for your body so we constantly need to correct this habit. You’ll need a regular reminder to pick your head up and move it back. Your muscles have become weak. You’ll need to build strength in the muscles at the top of the neck and you’ll need to revitalize the area at the top of your neck, creating a better environment for blood flow. You can do all this by simply moving your head back in line with the rest of your body. Movement creates lubrication for your joints. It helps them move more easily and smoothly. Instructions: Set an alarm for the top of the hour for each of your waking hours. I use an app called Simple Habit. I’m sure there are others. When the alarm goes off bring your chin back towards your body. Then return your chin forward over your body as far as it will comfortably go (this is a small movement overall). Then back your chin up towards your body as far as it will go. Repeat 10 times . Chin forward and chin back count as 1 time. Move within a comfortable range of motion. The movement is small and mindful. This is a sensitive area. Go slower than you think. If you have had the habit (and weakness) of dropping your chin forward, the top of your neck can feel rusty, thick, boggy, stiff, or dry. Be gentle. You’ll feel yourself move more easily as this area gets revitalized. When I first started doing this movement I felt like the top of my neck was rusty and that I was moving flakes of rust off with each movement. In a few days, with regular movement and mindful correction, my head moves much more smoothly on my neck and I’m able to move my neck farther in both directions (again this is a small motion). Slowly my neck is starting to feel longer like I’m working out the rust between the top few vertebrae (bones of the neck). Move gently, patiently and work within a pain free range of motion. Don’t rush this process. 4. Write down anything in your life that annoys you, or is bothering you then do something about it Why? Your nervous system likes when you take action to solve your problem, especially if you are prone to chronic fight/flight stress response. That response is all about movement and taking action. The action you take (no matter how small or big) is completing a biological process that signals to your nervous system to reset. The action could be small, like move your desk out from under that annoying air conditioner, or saying no when you don’t want to do something or it could be big like having that difficult conversation, or making a big decision like moving or changing jobs. If this is hard for you, practice taking little actions every day. It’s like training a muscle. The more you do it the easier it becomes, and it actually becomes energizing. I used to think I was a procrastinator until one day I realized I felt overwhelmed. If I did something about my situation, like make a phone call (which is hard for me) then I felt much better. I could finally relax. It was my body’s way of sending me a signal that I needed to take action to change my environment for a better feeling inside of my body. This is the point of this corrective. Instructions: In a journal make 4 columns (work, home, health, finances). Under work could think about your relationship with your boss, your colleagues, the physical environment, the vibe, the work you do, where your workstation is. At home you could include your house, your husband/partner, your kids, your pets, your neighbours, and your neighbourhood. Under health you can list your physical health, mental health, emotional health. Finances you can list your income and expenses. You get the idea. List stuff that’s relevant to you. Under each title write down anything that bothers you or doesn’t feel right for you. Include all the small stuff that annoys you and frustrates you and also include the big stuff. The point is to identify what doesn’t feel right for you. It doesn’t matter that it’s ok for someone else. Just because it feels right for someone else doesn’t mean it feels right for you. Don’t try to talk yourself out of or into something that doesn’t feel right for you. The point is if it doesn’t feel right for you, your body will interpret the stress as a threat and initiate a stress response which mean clenching and grinding your teeth, over activating the muscles of your jaw which causes you pain. Circle anything that bothers you from the above list that is within your control. There is always something you can do the make your life feel better for you. Take action daily to improve the environment of your life. 5. Cuddle with a loved one Why? Laying in stillness is our body’s most vulnerable time. Your body needs reassurance and reminders that it’s safe to lay in stillness. It needs to feel a sense of security and safety to sleep deeply. When we lay together in stillness with a loved one (partner, pet or child), especially with our naked skin touching their naked skin it stimulates the release of the hormone oxytocin which is involved in social bonding and love. For children and babies, laying in stillness with a parent makes them feel protected. Increasing a feeling of being safe decreases your body's need for defensive behaviors. Instructions: Lay together with a pet, partner, child or loved one. If you live alone and you don’t have a pet, surround one side of your body with pillows. You can be awake or fall asleep. If you are awake resist the urge to look at your phone or any other electronic device. Being still, present and responsive to each other is essential for your body to let go of the tension it holds to protect itself. Rest for 20-45 mins together. Try it first thing in the am, in the middle of the day or at night while going to bed. I like to do this early in the morning. I usually fall asleep as I lay with my husband and wake up feeling deeply rested. Thoroughly tested, these tools can help maintain your body in between sessions. Many of these are available for sale in my office, subject to availability. I do not receive any financial benefit from these companies for promoting these tools. It is recommended to get instruction from your LMT, PT, DC or Doctor before doing self massage.  Body massage ball - The best physio ball for creating more back flexibility, opening the chest and shoulders. Just the right amount of firmness, just the right size to stretch the back over or to place under your sacrum for a pelvic release. Cost: $20-30  Lacrosse ball or Knotty Body - It can be used to do cross fiber frictions in adhered areas, like the hip socket, bottom of feet, pectoralis minor and suboccipital areas. It also relieves trigger points, in particular in the trapezius and levator scapula muscles. Lacrosse balls are hard with rubber coating. Be careful when using them on the spine, for example, tied in a sock on either side of the spine. Tennis balls are great when the area is too tender or easily injured as they are significantly softer. The Knotty Body ball is in between a hard lacrosse ball and soft tennis ball. It is firm rubber with a hollow inside. Lacrosse balls and Knotty Body balls cost: $7-10  Theraband flexbar - Great for giving varied movements and therefore neuromuscular therapy to overly tight arms muscles. Many be helpful for tendonitis/tendonosis and/or carpal tunnel and other repetitive stress injuries of the lower arm and wrist. Cost: $20  Cupping set - It is best to receive instruction before cupping yourself as cupping can be harmful if not carefully applied. Yet, is an excellent way to release superficial adhesions and trigger points that keep coming back. It can be useful to purchase a set with the extension tube to help reach difficult areas. However, you may still need help placing the cups. Do not cup yourself frequently and check for contraindications. Hansol Bu-Hang is the brand I recommend for beginners. Cost: $29-45 Many people love their foam rollers and they have their place, but frankly myofascial release is the main reason people use them and they are not good at that. Instead of releasing fascia, they mostly crush it and roll right over it. From Massage Today
By James Waslaski Several weeks ago, after discussing my mother's "medical" condition with her surgeon, I realized how vital it is for our profession to establish the differences between medical and orthopedic massage. My mother had a critical medical condition called a dissecting aortic aneurysm, in which she exhibited low back pain symptoms, similar to someone with a tight iliopsoas. The medical doctor expected kidney problems, but - through divine intervention - an MRI discovered the massive aneurysm near the bifurcation of the femoral arteries, and it was ready to burst. I thank God each day that she did not go to someone minimally trained in medical or orthopedic massage, because an attempt to release her iliopsoas would have ruptured the aneurysm, and she likely would have died on the massage table. However, a year prior to discovering the aneurysm, my mother had an "orthopedic" condition called iliotibial band friction syndrome that presented as lateral right-knee pain; through the release of the gluteus maximus, the TFL, and other tight muscles around the knee, surgery was avoided, and she is pain-free one year later, thanks to proper stretching techniques. Iliopsoas Release Technique: This can place pressure on the abdominal aorta and iliac (femoral) arteries. Orthopedic massage involves therapeutic assessment, manipulation and movement of locomotor soft tissue to reduce pain and dysfunction. Restoring structural balance throughout the body allows us to focus on both prevention and rehabilitation of musculoskeletal dysfunctions. I hope for this to be one of many articles on the differences between orthopedic and medical massage so that there is more consistency within the profession on the use of the terms. It is my strong opinion that misusing the term "medical massage" will build a wall between massage therapists and other health care professionals who spend many years studying medical conditions that are quite different from orthopedic conditions. After spending almost 20 years in a trauma center, I have seen thousands of medical and orthopedic conditions. As massage therapists, there are several potential dilemmas we face when we claim to perform medical massage. For example:
I am concerned about organizations that claim to "certify" massage therapists in medical massage in as few as three days. Doctors - especially chiropractors - frequently ask me how a massage therapist with as little as 300-500 hours of training can become certified in assessing and treating medical conditions in one weekend. I tell them that many educators and therapists in our industry misuse the term "medical massage" because it is the current "buzz word." In other words, it sells seminars and sounds very clinical when used in practice and on business cards. But there are longer, more comprehensive massage programs out there that train students in medical settings and discuss the signs and symptoms of various medical conditions, and if you are already trained as a nurse, doctor, or in another medical specialty, you can see the big picture much more clearly. In my opinion, orthopedic massage is much more appropriate when we are treating musculoskeletal pain conditions or sports injuries. Its objectives are to restore structural balance in the muscle groups throughout the body, and decompress arthritic or painful joints. Muscle groups shorten, due to prolonged poor posture or repetitive motions, and shortened muscle groups need to be stretched out or they will pull bones onto nerves and blood vessels, and cause or contribute to all sorts of orthopedic conditions. I believe that conditions like joint arthritis are symptoms that result from tight muscles around a joint; thus, thoracic outlet and carpal tunnel syndrome are actually orthopedic conditions. In thoracic outlet, our goal is to lengthen short muscle groups, such as the anterior and posterior scalenes, the pectoralis minor, and any supporting muscles that compress nerves in the neck and shoulder and cause weakness and radiating pain into the arm or hand. Carpal tunnel can often be effectively treated by lengthening the pronator teres and the flexors of the wrist, and assuring the carpal bones are in alignment. Achilles tendonitis would be best addressed by lengthening the gastrocnemius and soleus muscles. In my opinion, it is truly orthopedic massage when we work to restore range-of-motion, balance out muscle groups surrounding the joints to treat pain, and work to prevent and rehabilitate injuries that involve muscles, bones, tendons and ligaments. Orthopedic massage is also great for performance enhancement. However, medical conditions can mask and/or complicate orthopedic conditions. For example, a woman in her third trimester of pregnancy may have excessive swelling in her wrists, adding to the tight muscles and tendons in the wrist area requiring medical assistance, perhaps also requiring the use of a diuretic (if not contraindicated) or lymphatic drainage to reduce inflammation. There are functional assessment tests that can determine most orthopedic conditions and outline a treatment plan using multiple modalities. These assessment skills better align you with other orthopedic experts, including orthopedic surgeons, chiropractors, physical therapists and osteopaths. I also believe that combining multiple disciplines allows better results. One patient may respond better to CranioSacral Therapy, while another requires lymphatic drainage, and the next needs a combination of myofascial release, neuromuscular therapy and stretching. (I will touch more on a multidisciplinary approach in a future article.) Lastly, patients need to be actively involved in their own treatment by perhaps changing the ergonomics of the work environment, watching their posture, using good body mechanics, and doing specific stretches and exercises between treatments. I would briefly like to address one other concern about the current state of the massage profession. I came from Florida and trained with many of the leaders in our industry. I also took college courses in pathology, biomechanics, anatomy and physiology, then took years of workshops to prevent "tunnel vision" into any one discipline from occurring. In Florida, the base training starts at 500-600 hours and becomes more advanced. In Texas (where I now live), a person can be a practicing and certified massage therapist with 300 hours. I recently attended a great insurance billing seminar here in Texas; what frustrated me, however, was that many of the attendees had only 300 hours of training. Even if these therapists learned to use the insurance billing codes properly, it is unlikely that after only 300 hours of training, they could ethically support their treatment and billing claims without additional training. I also see claims to "certify" these therapists in medical massage without administering a written and practical exam. No wonder the medical community looks down on us! I hope I have put a bit of fear into massage therapists that may still have a long way to go to understand that all medical conditions do not fall under plain and simple treatment protocols learned in a basic medical massage training program. As a profession, I suggest we work to distinguish medical conditions from orthopedic conditions to better align ourselves with other medical experts. I look forward to seeing how the National Certification Board for Therapeutic Massage and Bodywork defines an advanced-level therapist, once it moves to a higher level of certification, and is confident that the process includes a large panel of experts in role delineation and item-writing processes. I also hope that more schools and educators can agree on whether we should call our work clinical massage, orthopedic massage or simply an all-inclusive term like medical massage. |

 RSS Feed
RSS Feed
